Posts Tagged ‘New Fairfield Chiropractor’
Welcome to Chiropractic Life and Wellness Center's New Fairfield Chiropractor Archive. Here you can learn more about Chiropractic Life and Wellness Center, Chiropractic, and Dr. Brandon Chorney, today's choice for Chiropractors in New Fairfield, CT. Read Dr. Brandon Chorney's Chiropractic New Fairfield Chiropractor for the health of it.
We look forward to serving you! Call - 203-746-6543.
by Dr. Brandon Chorney | Jan 31, 2012 | Health Articles

Does it hurt when you chew, open wide to yawn or use your jaws? Do you have pain or soreness in front of the ear, in the jaw muscle, cheek, the teeth or the temples? Do you have pain or soreness in your teeth? Do your jaws make noises loud enough to bother you or...
Read More >>
by Dr. Brandon Chorney | Aug 2, 2011 | Health Articles

In the past, a patient presenting to a doctor with rheumatoid arthritis would not be told to “take a hike". First of all, that would have sounded rude, but as a genuine piece of advice it just didn’t figure in a doctor’s thoughts. Arthritis was looked on as a natural and unavoidable part of getting...
Read More >>
by Dr. Brandon Chorney | Jul 26, 2011 | Health Articles

If you have trouble sleeping, rest assured you are not the only one. Perhaps “rest assured” is the wrong phrase … Anyway, surveys into this problem reveal that between 40 and 60% of us don’t sleep as well as we’d like to. It may be down to money worries, family concerns, issues at work, aches...
Read More >>
by Dr. Brandon Chorney | Jun 28, 2011 | Health Articles

There will always be some bright spark inventing a new-fangled way to exercise. Strange machines and contraptions and weird exercise routines. If that sort of thing appeals, then fine - so long as it does what it’s meant to do. One thing you may not have considered, though, is simply getting back to basics in...
Read More >>
by Dr. Brandon Chorney | May 31, 2011 | Health Articles

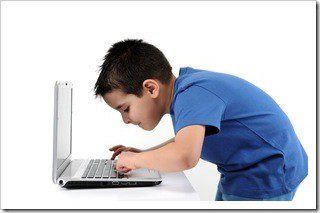
Good computer ergonomics – our posture when we sit at our workstations – is important for children as well as for adults. According to a New York Times article, over 70% of America’s 30 million elementary school students use computers. With the IT world we live in, the 30% that don’t soon will. While this is good for the minds of these children, it can be damaging to their bodies.
Doctors of chiropractic are treating more young patients who are suffering as a result of their working at ill-conceived computer stations – ill-conceived because they are designed for adults, or because they are poorly designed for children. It is a shocking thought, but many children already suffer from repetitive motion injuries (RMI), also known as repetitive strain injuries (RSI). One such injury is the problematic carpal tunnel syndrome. Chronic pain in the hands, back, neck and shoulders are other symptoms related to bad ergonomics.
Researchers from Cornell University published a study revealing that 40% of the elementary school children under their scrutiny were using computer workstations that created a postural risk. The other 60% were found to be in the range that raised “some concern.”
It is not enough to teach children how to use computers; more emphasis has to be placed on teaching them how to properly use the actual workstations. These are the formative years for an individual, mentally, emotionally and physically. Poor work habits when young can lead to serious health effects that plague that person for the rest of their life. While parents know to watch out for signs of substance abuse in their children, few have any idea of the long-term health effects that can arise from postural problems.
What can you do?
Thankfully, there are certain things you can do to lessen the chances of your child suffering painful and potentially disabling injuries:
- Make sure that any workstation in the home that is shared by both adult and child can be modified according to the user.
- Check that the top of the computer monitor is set at a height at or below the child’s eye level. You may need to remove the monitor stand to do this, or alternatively raise the child’s sitting position in some way.
- Look at the workstation chair and ensure it is correct for the child. To stop slouching and for added back support, you can place an ergonomic back cushion, a pillow or a rolled-up towel in a position that corresponds with the small of the child’s back. Make sure that the gap between the front edge of the seat and the back of the knees is two inches. A good workstation chair should have arm supports that cause the elbows to rest at an angle between 70 to 135 degrees relative to the computer keyboard.
- Check that the wrists are held in a neutral position while typing, and not angled up or down. To ensure the child doesn’t have to hold their arm out away from their body, move the mouse mat close to the keyboard.
- Achieve a 90- to 120-degree angle for the child’s knees, if necessary by installing a foot rest, or perhaps a box or a small stool.
- Ensure there is adequate lighting to reduce eyestrain, and check the monitor is not reflecting any glare. Use a special antiglare screen if necessary.
- Do not allow your child to sit for uninterrupted hours at the computer. Limit their time, and enforce breaks during which they can stretch and move about. Have them perform the following stretches: clench the hands into fists and move them in 10 circles inward, followed by 10 circles outward; place hands in a praying position and squeeze together for 10 seconds, then point them downward and do the same squeezing for another 10 seconds; spread the fingers apart, then close them one at a time; stand and have them wrap their arms around the body, turning all the way round to the left, then all the way round to the right.
- Try to have your child drink four 8-ounce glasses of water every day so their muscles and all their bodily functions are adequately hydrated. This can help avoid injury. Juices and sodas etc. are not a suitable replacement for water.
- Suggest to your child’s school and PTA that the children are educated on proper computer ergonomics, and encourage the installation of ergonomically correct workstations at the school.
If you or your child continue to suffer from computer-related pain despite your best efforts to avoid it, your next stop should be a doctor of chiropractic to prevent the injury worsening and to promote healing.